What is a brain aneurysm?
A brain aneurysm is a balloon-like swelling that results from a weakness in the wall of one of the blood vessels supplying blood to the brain. There is a risk that the aneurysm will rupture (burst suddenly) and cause a haemorrhage (bleed).
What is coiling?
In the 1990s, coiling was introduced as a way of treating ruptured and unruptured brain aneurysms without the need for a craniotomy (an operation that opens the skull to expose the brain). (You may wish to see our fact sheet, Craniotomy, for further information.) Coiling involves approaching the aneurysm from inside the blood vessel, so that there is no need to open the skull. Small metal coils are inserted into the aneurysm through the arteries that run from the groin to the brain. The coils remain in the aneurysm; they are not removed. They stop blood flowing into the aneurysm and therefore reduce the risk of a bleed or a re-bleed.
What happens before the procedure?
The coiling procedure is similar to an angiogram (an X-ray test to take pictures of the blood vessels) and involves a very small tube, called a ‘catheter’, being guided from the groin up to the brain through the blood vessels. However, it is a much more complex procedure and is always carried out under a general anaesthetic in the radiology department.
You must not eat or drink anything for four to six hours before the procedure. The staff on the ward will advise you on this.
On arrival at the radiology department, an anaesthetist will give you a general anaesthetic, so you will be asleep throughout the procedure.
What happens during the procedure?
The room will have several large pieces of high-tech scanning equipment which are needed to perform the coiling.
A nurse will shave a small area of your groin where the catheter will be inserted.
The radiologist (a doctor specially trained in radiology) will make a small incision (cut) in your groin through which they will insert the catheter into the main blood vessel in your leg (the femoral artery). The catheter is then guided through other blood vessels in your body until it reaches your brain and then the aneurysm.
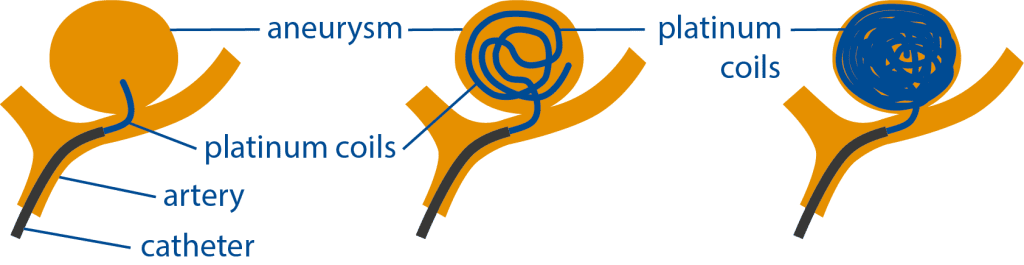
The coils are passed through the catheter and, one by one, they are slowly inserted into the aneurysm. The coils are made of platinum, are twice the width of a human hair and can vary in length. The number of coils needed depends on the size of the aneurysm. The largest coil is inserted first and then smaller coils are inserted until the aneurysm is filled. Usually, several coils will be used.
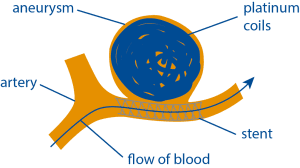
Sometimes, an expandable mesh tube, called a stent, may also be put into the artery to hold the coils in place inside the aneurysm. This is called stent-assisted coiling. It is more likely to be done if the aneurysm has a very wide ‘neck’ (where the aneurysm meets the artery) that could otherwise allow the coils to escape.
There are different types of stents, and different techniques that use stents, and not all use coiling as well. The types of stents and techniques are advancing all the time. If a stent is used, you will have to start lifelong antiplatelet (blood thinning) medication. You should never stop taking this medication, unless your doctor advises you otherwise.
Once the coils are in place, the radiologist will remove the catheter. The opening in your artery in your groin may be closed using a very small ‘plug’ called a vascular closure device. The area of your groin might be slightly painful afterwards and there may be some bruising.
Coiling is a complex and delicate procedure that will take at least three hours and often longer.
What happens after the procedure?
You will probably spend some time in the recovery room – usually at least two hours. During this time, regular neurological observations will be performed by the nursing staff. This is to check that you are waking up properly from the anaesthetic. It involves asking you simple questions, testing the strength of your arms and legs and shining a light in your eyes. Your blood pressure, heart rate, respiratory rate and oxygen levels will also be monitored.
The nurse will check the small wound in your groin for any bleeding and also check the pulse in your foot. This is to ensure that your blood circulation to your leg has not been affected.
You may need to lie flat for a time following the procedure to help with your blood pressure and reduce the chance of bleeding at the puncture site in your groin. However, this won’t always be necessary. The nurses will tell you what you should do.
Throughout this time, the nurses on the ward will continue to monitor you and carry out neurological observations. Painkillers will be given for any discomfort or headaches you might be experiencing. You are also likely to have a drip to prevent dehydration and possibly a urinary catheter (a tube that empties the bladder of urine so you don’t need to get up to use the toilet). Because you are restricted to bed rest, you will have to wear pressure stockings to help prevent blood clots forming in your legs (deep vein thrombosis).
Some people experience mild groin discomfort for a short time after the procedure around where the catheter was inserted. Most people make a relatively quick recovery from elective coiling.
Can the coils move?
Once the coils are securely in place they are extremely unlikely to move out of the aneurysm. However, they might settle and become more compact over time, leaving space within the aneurysm. This might mean that more coils are required to block off the aneurysm fully. Around one in 10 patients will require further treatment.
Any follow-up after the procedure will be decided on an individual basis. You may have follow-up scanning after coiling, although this isn’t necessary for some people. Your consultant or specialist will discuss this with you.
What are the risks of coiling?
The levels of risk will very much depend on your own individual circumstances, including the size and location of the aneurysm in your brain, whether or not it has ruptured (burst), your age and your overall health.
It is likely that the benefits of coiling will strongly outweigh any possible risks, and your doctor will have discussed this with you fully before you give your consent to go ahead with the procedure.
However, as with any invasive procedure, there are possible complications. These include stroke-like symptoms, such as weakness or numbness in an arm or leg and problems with speech or vision.
There is also a risk of bleeding, infection or damage to the artery at the place where the catheter goes into your groin.
Based upon the evidence available, doctors agree that coiling is a safe procedure.
How successful is coiling?
Research is still exploring the benefits and risks of coiling. Various studies have been published. The largest is the International Subarachnoid Aneurysm Trial (ISAT). This trial was designed to explore how effective coiling is compared to craniotomy and clipping for ruptured aneurysms. The trial involved different neurosurgical centres and a total of 2,143 patients took part. The ISAT trial showed that the long-term risks of further bleeding are low for both coiling and clipping. The results supported using coiling as a treatment for ruptured aneurysms, because it offered better survival rates and reduced risk of long-term disability for patients.
About this page
This fact sheet provides information on elective coiling for brain aneurysms. Our fact sheets are designed as general introductions to each subject and are intended to be concise. Each person is affected differently and you should speak with your doctor or specialist for individual advice.